Living on a fixed income is hard, which is why many Americans depend on Medicare to help with medical expenses. But Medicare isn’t static, and it’s important to stay up to date with changes, whether you’re on Medicare yourself or care for someone on Medicare.
For You: Apple Is Making Low-Cost Hearing Aids — Here’s How Retirees Can Take Advantage
Learn More: 9 Easy Ways To Build Wealth That Will Last Through Retirement
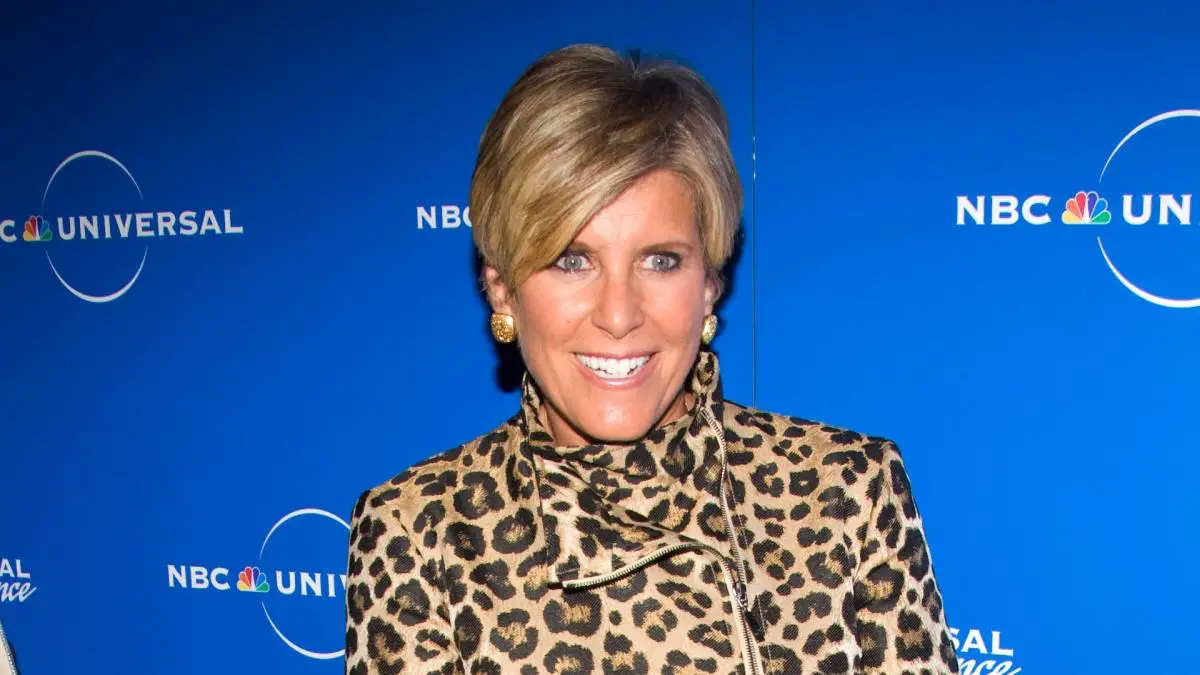
Personal finance expert Suze Orman stressed the importance of staying on top of developments with Medicare in a post to her personal blog. Specifically, Orman says there are two important Medicare issues you need to be aware of and address today.
Read on to learn of these important developments and what you need to know to navigate the Medicare system.
It’s Going Viral: Want to Retire Rich? Suze Orman Says You’re Missing This Key Money Move
In her post, Orman said that anyone enrolled in a Medicare Advantage plan typically needs to get pre-authorized approval for major care costs. If an insurer denies a preauthorization request, however, that doesn’t mean it’s a hard no.
Orman cited a study by the Kaiser Family Foundation (KFF) that found when patients appealed an initial denial, the insurer reversed its decision in more than 80% of cases after appeal.
There’s a clear reason for this. Insurers often must cover these costs to honor Medicare Advantage policies, but the same KFF study found that just 10% of people file appeals after being denied coverage.
Denying coverage in the first place is a simple way for the insurance company to hope the insured just goes away, saving the company money. After all, actually paying for health services cuts into the business’s bottom line.
Whether you’re on a Medicare Advantage plan or you’re caring for an adult on one, it’s crucial to remember that “no” doesn’t always mean “no” when it comes to insurers. If coverage was denied once, there’s a good chance the insurer will change its mind after appeal.
Read Next: I’m Retired and Regret My Frugal Retirement — Here’s Why
Beginning in January 2025, there will be a $2,000 cap on what Medicare enrollees must pay out of pocket for prescription drug costs. This change should save the majority of Medicare patients who access prescriptions through their plan a good deal of money. However, even those savings will come at a cost.
This new cap is also expected to cause insurance companies to increase monthly premiums for Part D prescription drug plans. Orman suggested it may even cause insurers to change their rules on what drugs they’re willing to cover.

Leave a Comment