Gabrielle Goodrick’s day has barely begun and she’s already poring over a stack of legal documents. As the nurses and other doctors at her clinic start seeing the first of what will be upwards of 40 patients that day, the 59-year-old family medicine doctor and owner of Camelback Family Planning – one of Arizona’s few abortion clinics – has a decision to make.
Since the supreme court overturned Roe v Wade in June 2022, Arizona has banned all abortions after 15 weeks of pregnancy – with a small but vague carveout for medical emergencies. In November, Arizona voters will get to weigh in on a ballot measure that would enshrine the right to abortion until viability, or around 24 weeks.
But that ballot initiative won’t help the 32-year-old woman in Goodrick’s waiting room. The woman had been thrilled five months ago when she’d gotten pregnant, seven years after the birth of her first child, until her water broke prematurely 17 weeks into her pregnancy – far too early for her baby to survive. With no amniotic fluid left in her uterus, it’s only a matter of time until an infection sets in.
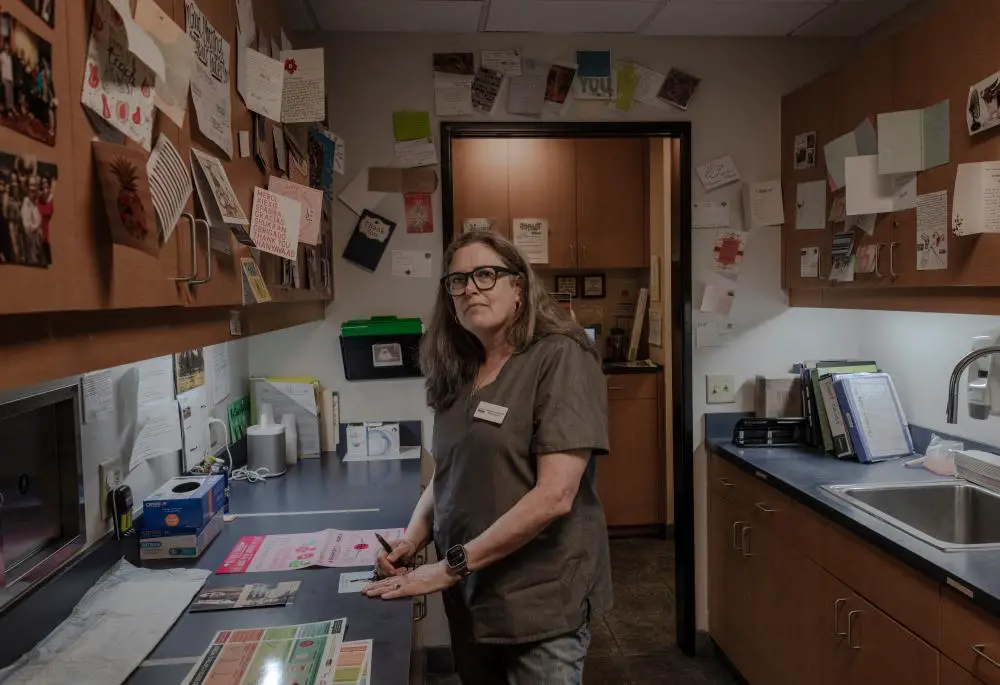
In the clinic’s break room, Goodrick sets down the stack of papers – which include a letter four state representatives wrote to Arizona’s attorney general this summer asking what qualified as a “medical emergency” and the attorney general’s response. Dressed in turquoise corduroy trousers and a white button-up, Goodrick pulls her hair into a claw clip before she begins describing the case to a few of the clinic’s nurses. Across the room, her colleague Barbara Zipkin, an obstetrician-gynecologist, listens in as she strokes her 5lb, 16-year-old dog Scooter. The Maltese-Yorkie mix is a fixture at the clinic, regularly accompanying Zipkin into patient rooms to provide emotional support.
“No one will do it,” Goodrick says. So far, the only known abortions after 15 weeks in the state have been performed when a patient develops a severe infection, but Goodrick doesn’t want to make this patient wait that long.
The woman’s healthcare network has already said it won’t end the pregnancy, and so she and her husband have started talking to a doctor in Las Vegas. But the six-hour drive to Nevada is no small hurdle. And that clinic – like most offering abortion care in the second and third trimester in the United States – only offers a procedure called dilation and evacuation. During a D&E, a patient’s cervix is dilated, often using small rods called laminaria that slowly expand over the course of one to two days, before a doctor empties the patient’s uterus using suction or surgical instruments. It’s difficult for providers to remove the fetus intact during a D&E – but this woman wants to hold her baby to say goodbye.
Camelback is one of only a handful of clinics in the US offering an alternative called induction abortion. Like a medication abortion, in which patients take the abortion pills mifepristone and misoprostol to end a pregnancy in the first trimester, an induction abortion involves taking the same pills in the second or third trimester. Because the fetus is larger than in the first trimester, the misoprostol triggers contractions that are more akin to labor than an earlier medication abortion, and the procedure usually occurs in a hospital instead of at home. (Camelback manages the pain of that labor – which is quicker and less severe than childbirth – with painkillers and conscious sedation). The result is that patients – like this one – can hold and grieve the fetus afterwards, and even take home footprints.
There’s legal risk to helping this patient – Goodrick’s not sure she would do it if the state didn’t have a Democratic governor and attorney general – but she’ll remark later how frustrating she finds it that more doctors aren’t willing to use their position to more aggressively challenge abortion restrictions. She is in a bind countless doctors have faced in the last two years, as stories of women denied emergency abortions in their home states have piled up.
Zipkin agrees they need to act. From her perch on a black office chair, she responds, defiant: “I’m not afraid. Let’s do it.”
***
In the aftermath of Roe, patients across the United States are seeking abortion care later in pregnancy, as a growing web of restrictions makes it increasingly difficult for them to access care sooner. And the procedure most physicians offer after the first trimester, a D&E, is not always the procedure patients want – for example, if they’d prefer to hold their fetus after or avoid cervical dilation with laminaria.
When she found out that we could see her, she started crying. She was just overwhelmingly relieved
In the United States, abortion pills are FDA-approved through 10 weeks of pregnancy – but it’s still legal to use them “off label” later. While they’re not widely prescribed later in the US, they are the standard for second- and third-trimester care in much of northern Europe – and the World Health Organization’s abortion care guidelines describe how to use the pills up to and beyond 24 weeks of pregnancy.
Goodrick and her colleagues are hopeful that educating more physicians on the use of abortion pills later in pregnancy could expand access to care across the US by allowing more physicians with labor and delivery training, rather than only doctors with the surgical skills required to perform a D&E, to offer the procedure. Although conservative groups have called the abortion pill “unsafe” in an attempt to undo the FDA’s approval of the medication, Goodrick believes it could be an equalizer for physicians.
In that spirit, this year they published a study sharing their experience providing hundreds of induction abortions to end pregnancies between 18 and 24 weeks before Roe fell. They also regularly host and train medical students.
Offering that care has been harder – but not impossible – since Arizona banned abortions after 15 weeks. Since the ban went into effect, Camelback has directed patients whose pregnancies are past that mark to a clinic in southern California, where they’re able to receive and take mifepristone, which stops the pregnancy from progressing. The next day, after they’ve returned to Arizona, Goodrick and her team administer misoprostol, which induces contractions. They’re able to do so because the pregnancy has already ended, Goodrick says, meaning they’re essentially treating a stillbirth. It’s a loophole that Goodrick’s attorneys have reassured her is legal – and it helps patients avoid the cost of a surgical procedure and out-of-state hotel.
But this patient, who has found her way to Camelback one day in mid-September, is the first the clinic will treat entirely in Arizona since the state’s 15-week ban went into effect in 2022.
“When she found out that we could see her, she started crying,” Goodrick said. “She was so upset still about the hospital not helping her. She was just overwhelmingly relieved.”
“I know it’s scary” for doctors to push back against restrictions, says Goodrick – and she understands that hospitals and their legal teams are even more risk averse. But she’s steadfast: “I think it’s up to the medical field to say [to the state], ‘You don’t know what you’re talking about.’”
***
Goodrick never intended to provide abortion care – but early in her career she saw the need.
She remembers Henry Morgentaler’s name appearing in the news when she was an undergraduate student at McGill University in Montreal in the 1980s. A Holocaust survivor, Morgentaler had emigrated to Canada, where he began his career, like Goodrick, as a general practitioner. Over time, he became one of the first Canadian doctors to offer vasectomies, IUDs, birth control to unmarried women, and eventually abortions – and his repeated challenges of Canadian law would lead to abortion being legalized nationwide in 1988. The next year, Goodrick enrolled in medical school.
At the University of Vermont, Goodrick felt drawn to women’s health – but not obstetrics and gynecology, a surgical specialty. Instead, she gravitated toward family medicine, where she could receive some obstetrics training but follow patients through their full lives. In 1990 anti-abortion protesters descended on Burlington with the intention of closing two clinics there. That year, she co-founded a pro-choice alliance of medical students at the university.
“I didn’t really think of abortions like, ‘This is what I’m going to do,’” she said. But when Goodrick began her residency at Phoenix Baptist hospital (now Abrazo Central) in 1993, she did a rotation at the local Planned Parenthood and enjoyed it. She would ultimately open a family practice clinic, where she also offered occasional abortions, though they weren’t the focus of her work.
That changed after 2000, when the Food and Drug Administration approved mifepristone for use in the US. Goodrick says she was the first provider in the south-west to offer the abortion pill – and she remembers patients flying in from across the country to access it.
In those years, even though Roe was still standing, there were few physicians providing second-trimester abortions in the US, and one of the most prominent, George Tiller, was murdered in 2009. As she developed her skills in D&E, Goodrick began to wonder, “How am I going to get help? How am I going to be doing this five days a week for the rest of my life?” The surgical procedure required advanced training, and she worried about finding other physicians to fill in at and eventually take over her practice.
In 2018, Goodrick was attending the International Federation of Abortion and Contraception Professionals’ biannual conference in France when she walked into a session led by Swedish midwives. She discovered that it’s standard in Sweden to provide second trimester abortions not with surgical instruments, but with pills.
“We VERY rarely use D&E and almost exclusively use medical abortion”, or pills, in Sweden, said Kristina Gemzell Danielsson, a professor of obstetrics and gynecology at the Karolinska Institutet in Stockholm, via email. In the 1980s, she helped develop what would become the WHO protocol for using abortion pills in the second trimester.
“Due to our geography and [the fact] that many live far from a hospital, surgical abortion in the second trimester is not feasible,” she said. Today, medication abortion in the second trimester, a rarity in the US, is available “in all OB-GYN clinics in the whole country”, she adds. It is often performed by midwives.
When Goodrick returned to Arizona, she told the doctors at her clinic she wanted to bring the practice to the clinic. They were wary at first. D&Es had been in use in the US since the 1970s and were by far the most common way to end a pregnancy in the second trimester; today, they make up about 95% of abortions after 14 weeks in the US. Studies in the late 2000s had found that D&Es resulted in fewer complications than inductions (though research today suggests they’re equally safe) and many providers preferred a 20-minute procedure to hours-long labor.
But Zipkin would get on board and today prefers the inductions. While the risk of perforating the uterus with surgical instruments during a D&E is low, with induction abortions it disappears – and patients don’t have to spend the day before in discomfort as laminaria dilates their cervix.
Although training in D&E is still vital for any clinic offering care later in pregnancy – in case, for example, a patient’s uterus doesn’t expel all of the pregnancy tissue with pills alone – Goodrick believes the medication might allow more providers to offer abortions in areas where OB-GYNs are few and far between.
***
Related: Where will abortion be on the ballot in the 2024 US election?
There are about half a dozen protesters outside Camelback when Goodrick returns to work the morning after meeting with the patient who needs help as her pregnancy approaches 20 weeks. The sight isn’t unusual, and Goodrick notes that they’ll be gone by the time the Arizona sun is high in the sky, pushing temperatures into the 90s on this relatively cool summer day. Two cheerful clinic escorts greet patients at their cars and use large umbrellas to block them from the protesters’ views.
As she holds the clinic door open for patients, one of the escorts – a 66-year-old sporting a rainbow vest, straw witch’s hat and a bevy of buttons and pins promoting feminism and voting rights – recalls the second-trimester abortion she received in 1999. She’d been trying to get pregnant and, at one of her regular prenatal appointments, her doctor realized her fetus had stopped growing, probably two weeks earlier. Her regular OB-GYN had been able to offer her a D&E. “Now in Arizona I would not be able to do that,” she says, declining to give her name.
The 32-year-old mother in need of care is now resting in a recliner inside. When she arrived at the clinic that morning, Zipkin gave her a small dose of misoprostol to induce labor and painkillers to ease the ensuing cramps. By lunchtime, when Zipkin sits down to sip an orange Sunkist, it’s delivery time: “Doctor!” a nurse beckons down the hall. Within a few minutes, Goodrick joins her in the patient’s room.
Less than an hour later, they’re both back in the break room. The woman is coming out from under sedation; her husband is about to join her to say goodbye to their baby. “She did great,” Zipkin says.
Goodrick has by now spoken with the Arizona attorney general, who has reassured her the case falls under her definition of a medical emergency. But she worries the Arizona department of health will still flag the case after Camelback reports it – and that the conservative county attorney could decide to prosecute the clinic despite the state AG’s position.
She’s hopeful she won’t have to deal with these kinds of concerns after Arizonians vote in November on whether to enshrine the right to abortion until 24 weeks. “Obviously what happens federally is very important, but every state needs their own ballot initiative,” Goodrick said.
In moments like these, Goodrick reflects on the legacies of abortion providers who came before, like Dr Tiller. “A lot of us still think of him. ‘What would he do now? How would he act? How would he be calm and sure of himself?’” she says.
It’s why, she says, she told the attorney general, “In the future, if you hear of these cases and they can’t get done in the hospital, tell us. We’ll see them.”

Leave a Comment